Antibody-drug conjugates (ADCs) represent the next frontier in targeted cancer therapies, combining the specificity of monoclonal antibodies with the potency of cytotoxic drugs. One of the most critical components in the construction of effective ADCs is the linker technology, which serves as a bridge between the antibody and the cytotoxin. A deep dive into ADC linkers reveals the complexities behind the development of ADC linkers and their conjugation with cytotoxins, leading to promising advancements in oncology.
What are ADCs?
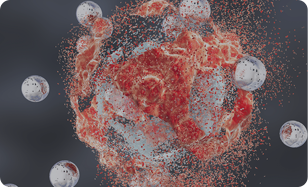
ADCs are sophisticated therapeutic agents designed to selectively deliver cytotoxic drugs to cancer cells while sparing healthy tissues. This selectivity is achieved through the targeted nature of antibodies, which can bind to specific antigens overexpressed on cancer cells. The role of the linker is pivotal, as it must ensure that the cytotoxin is effectively delivered to the tumor site while remaining stable in circulation.
The Role of ADC Linkers
ADCs typically consist of three main components: the antibody, the cytotoxin, and the linker. The linker is a chemical structure that connects the antibody to the cytotoxin and plays a crucial role in:
Stability: The linker must be stable in the bloodstream to prevent premature release of the cytotoxic agent.
Release Mechanism: Upon reaching the target cell, the linker should allow for the release of the cytotoxin within the cancer cell, often triggered by specific conditions, such as pH changes or enzymatic cleavage.
Toxicity Reduction: Effective linkers minimize systemic toxicity by ensuring that cytotoxins remain inactive until they are internalized by the target cell.
ADCs Cytotoxin with Linkers
The efficacy of ADCs significantly depends on the choice of cytotoxins and linkers. Commonly used cytotoxins include microtubule inhibitors like maytansinoids and auristatins, which require effective linkers for successful conjugation. The design of these linkers affects the overall therapeutic window of ADCs. For instance, cleavable linkers can provide an efficient release of the cytotoxin within the target cells, allowing for a potent anticancer effect, while providing reduced toxicity to normal cells.
ADC Linker Development
Recent advances in ADC linker development focus on optimizing the balance between linker stability, drug release kinetics, and overall bio-distribution. Researchers are exploring several types of linkers:
Cleavable Linkers: These linkers are designed to break down within the cancer cell environment, typically under acidic conditions or via hydrolysis, releasing the active cytotoxin only within the tumor.
Choosing the right linker can lead to customized ADCs tailored for different types of cancers, enhancing their therapeutic efficacy while minimizing side effects.
ADC Linker and Cytotoxin Conjugations
The actual process of conjugating linkers to cytotoxins and antibodies is critical in ADC development. Different conjugation strategies include:
Site-Specific Conjugation: This method involves attaching the linker at specific locations on the antibody, thus preserving the antibody’s biological activity and ensuring predictable pharmacokinetics.
Random Conjugation: While simpler and less costly, random conjugation can lead to heterogeneous populations of ADCs that may have variable efficacy and safety profiles.
Through site-specific conjugation and innovative linker designs, researchers have been able to significantly enhance the potency of ADCs from a mere therapeutic tool to a powerful weapon against malignancies.
Conclusion
The future of cancer therapy lies in the successful development of ADCs, where the ADC linkers play an indispensable role in determining their efficacy and safety. As research continues to evolve, particularly in the field of ADCs cytotoxin with linkers, we can anticipate novel treatments that not only improve patient outcomes but also redefine the standards of care in oncology. Understanding ADC linker technologies and their application in cytotoxin conjugations will be crucial in leading the charge against cancer and enhancing the clinical landscape of targeted therapies.