Angioedema is a medical condition characterized by sudden swelling beneath the skin or mucous membranes. It often appears around the eyes, lips, tongue, throat, hands, or feet and can sometimes become a life-threatening emergency if the airway is compromised. Understanding the causes, risk factors, and treatment options for angioedema is crucial for patients, caregivers, and healthcare professionals.
Understanding Angioedema
Angioedema is similar to hives (urticaria), but while hives affect the surface of the skin, angioedema occurs in deeper layers. The swelling develops due to fluid leaking from blood vessels into surrounding tissues, often triggered by an immune system response. Depending on the underlying cause, angioedema may be classified into different types
-
Allergic angioedema Caused by exposure to allergens such as foods, insect stings, medications, or latex.
-
Drug-induced angioedema Triggered by certain medications, including antibiotics, pain relievers, and blood pressure drugs.
-
Hereditary angioedema (HAE) A rare genetic disorder involving a deficiency or dysfunction of the C1 esterase inhibitor protein.
-
Acquired angioedema Similar to HAE but develops later in life, often linked to autoimmune or lymphoproliferative conditions.
-
Idiopathic angioedema When no clear cause can be identified.
Common Causes of Angioedema
1. Allergic Reactions
One of the most frequent causes is an allergic reaction. Common triggers include:
-
Foods such as shellfish, peanuts, eggs, and milk
-
Insect bites or stings
-
Environmental allergens like pollen or animal dander
-
Medications, including antibiotics like penicillin or even cephalexin capsules in rare cases
When the immune system detects an allergen, it releases histamine and other chemicals that cause fluid to leak into tissues, resulting in swelling.
2. Medication-Induced Angioedema
Many drugs are associated with angioedema. For example:
-
ACE inhibitors (used to treat high blood pressure) are a well-known cause.
-
Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen may also trigger swelling.
-
Antibiotics, including cephalexin capsules, can rarely cause allergic angioedema. Although cephalexin is commonly prescribed for bacterial infections like skin infections and urinary tract infections, patients with penicillin allergies may react adversely.
3. Genetic Factors
Hereditary angioedema is less common but more severe. It results from a defect in the C1 esterase inhibitor gene, leading to uncontrolled inflammation and swelling. Unlike allergic angioedema, it does not respond well to antihistamines or corticosteroids.
4. Autoimmune and Idiopathic Triggers
Some cases of angioedema are linked to autoimmune conditions such as lupus. In idiopathic angioedema, no cause is identified, but patients may still experience recurrent swelling episodes.
Symptoms of Angioedema
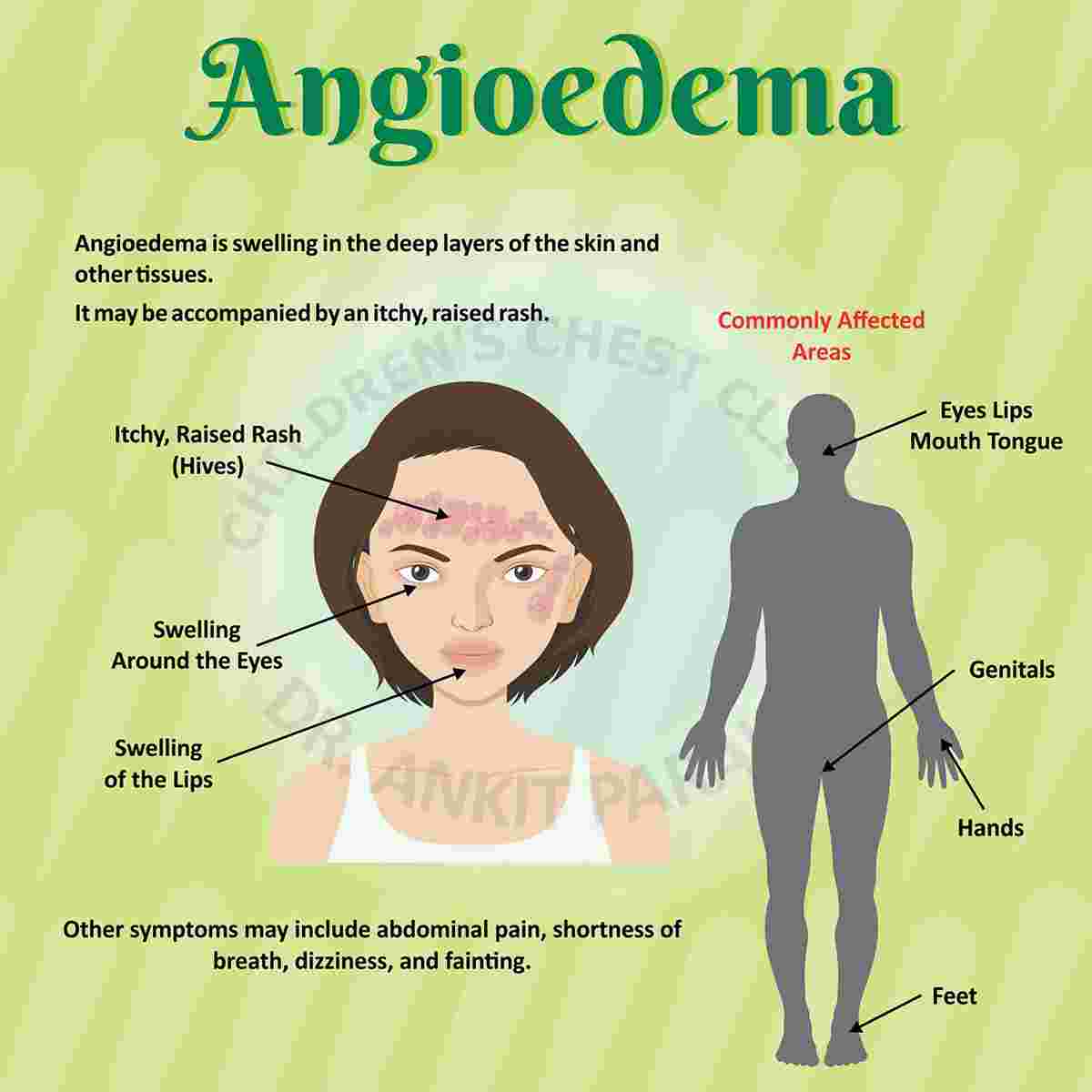
Symptoms vary depending on the location and severity of swelling. Common signs include
-
Rapid swelling under the skin, especially around the face, lips, eyes, and throat
-
Swollen hands, feet, or genitals
-
Abdominal pain, nausea, and diarrhea in gastrointestinal angioedema
-
Difficulty breathing or swallowing in severe cases
Severe airway involvement requires immediate emergency treatment since it can lead to suffocation.
Diagnosis of Angioedema
A doctor will typically begin with a detailed medical history and physical examination. Important diagnostic steps include
-
Review of medications determining if drugs such as ACE inhibitors or antibiotics like cephalexin capsules could be involved.
-
Allergy testing skin prick tests or blood tests may identify specific allergens.
-
Genetic testing if hereditary angioedema is suspected.
-
Blood tests to evaluate levels of C1 esterase inhibitor and complement proteins.
Treatment of Angioedema
The treatment of angioedema depends on the underlying cause. Options range from immediate emergency care to long-term preventive therapies.
1. Emergency Treatment
If angioedema affects breathing or swallowing, it becomes a medical emergency. Urgent interventions may include:
-
Epinephrine (adrenaline) injection to reduce swelling and open airways
-
Oxygen therapy
-
Intubation or tracheotomy in life-threatening airway obstruction
2. Medications for Allergic Angioedema
-
Antihistamines (such as cetirizine or diphenhydramine) reduce histamine activity.
-
Corticosteroids (prednisone or hydrocortisone) help control inflammation.
-
Epinephrine auto-injectors (EpiPen) are prescribed for individuals with a history of severe allergic reactions.
If a patient reacts to an antibiotic such as cephalexin capsules, the medication should be discontinued immediately and replaced with an alternative that does not trigger allergic responses.
3. Treatment for Hereditary Angioedema
-
C1 esterase inhibitor concentrates (administered intravenously) help restore deficient protein levels.
-
Bradykinin receptor antagonists such as icatibant can control attacks.
-
Long-term prophylaxis may involve medications like androgens (danazol) or modern biologics to reduce frequency of attacks.
4. Lifestyle and Preventive Measures
-
Identifying and avoiding triggers such as certain foods, medications, or environmental factors.
-
Wearing a medical alert bracelet to inform healthcare providers of the condition.
-
For those with a history of drug-induced angioedema (e.g., reaction to cephalexin capsules), keeping a record of allergy information is critical.
The Role of Cephalexin Capsules in Angioedema
Cephalexin capsules are widely used to treat bacterial infections, including respiratory infections, skin infections, ear infections, and urinary tract infections. While effective and generally safe, cephalexin like other beta-lactam antibiotics can trigger allergic reactions in sensitive individuals.
How Cephalexin May Cause Angioedema
-
Allergic Reaction: In some patients, the immune system mistakenly identifies cephalexin as harmful, leading to histamine release and swelling.
-
Cross-Reactivity with Penicillin: People allergic to penicillin may also react to cephalosporins like cephalexin.
-
Severe Cases: Rarely, angioedema caused by cephalexin capsules can escalate to anaphylaxis, a potentially fatal reaction requiring immediate epinephrine treatment.
Safety Measures
-
Patients with known allergies should inform healthcare providers before starting cephalexin.
-
Physicians often recommend allergy testing or alternative antibiotics if there is a history of beta-lactam hypersensitivity.
-
If angioedema occurs while taking cephalexin capsules, the drug should be discontinued, and emergency medical attention should be sought.
Long-Term Outlook for Angioedema Patients
Most patients with allergic or drug-induced angioedema recover fully once the trigger is identified and avoided. For hereditary angioedema, lifelong management is required, but new therapies have improved patient outcomes significantly. Preventive care, patient education, and prompt emergency treatment remain key to controlling this condition.
Conclusion
Angioedema is a complex condition with multiple possible causes, ranging from allergic reactions and drug sensitivities to genetic disorders. Recognizing symptoms early and seeking appropriate treatment can be lifesaving, especially when the airway is compromised.
Medications like cephalexin capsules, though widely prescribed and effective, can occasionally trigger allergic angioedema. Patients should always discuss their medical history and any known allergies with their healthcare provider before starting new medications.
With accurate diagnosis, targeted treatment, and preventive strategies, angioedema can be effectively managed, allowing individuals to live healthier and safer lives.